Bait and Switch
New labels are being proposed to identify “healthy” foods. Maybe we should also stick a scarlet U on ultra-processed foods, now blamed for obesity, childhood metabolic diseases – even society’s general downfall? A closer look indicates that causal relationships between UPFs and juvenile metabolic diseases are far more nuanced than currently touted, with exacerbating, contributing, and alternative risk factors tangling the causal chain. Before policy decisions remove/limit these products from market shelves, a better understanding of mechanisms fostering consumption, clarification of the causal chain, and a calculation of deaths and illnesses that would be prevented by proposed responses are warranted. That means more research must be done. It also means deflecting attention from infectious disease and death prevention is misguided. [1]
It bears mention that Senators were coopted and deflected from focusing on Kennedy’s past promulgation of anti-vax propaganda when he substituted a different sacrifice to his senatorial superiors, misdirecting them to spending the next 8 years countering obesity and other chronic diseases while ignoring his attachment to the fake autism-vaccine connection.
Numerous hypothesis-generating alternative causes and confounding factors for obesity and metabolic diseases, e.g., Type 2 diabetes and fatty liver, especially in children, have been discovered that warrant further investigation before we can believe that RFKJr’s approach will MAHA. Here are some:
What’s the Addiction Trigger?
The mass cessation of cigarette smoking, beginning in 1964, tracks the weight gain trend. This, of course, is a correlation. However, as anyone who has stopped smoking will tell you, smoking cessation is usually accompanied by weight gain – if you don’t smoke, you eat. As one review stated,
“…smoking cessation in the absence of nicotine replacement therapy typically results in significant and sustained hyperphagia [an extreme craving for food] and weight gain.”
Could the onslaught of obesity be triggered by craving an alternative to nicotine, such as food, rather than some mechanism triggered by UPF? Do ex-smokers preferentially consume unprocessed foods or UPFs? Sadly, no one knows. The research is ambivalent at best, often conflating the connection between UPF, obesity, morbidity, and Non-Alcoholic Fatty Liver Disease (NAFLD), a classic indication that identifying confounders has not been addressed.
One 2023 study claimed to be the first to report a positive association between UPF and NAFLD in teens controlled for age, sex, race/ethnicity, and educational attainment. Neither cigarette smoking nor other possible confounders were included, making their conclusions tenuous. Further, the authors report studies with conflicting and even negative results.
And, while proponents of the UPFs-addiction theory contend, with limited evidence, that these foods coopt the neurotransmitter reward system, there is potentially competing evidence that carb craving is partially genetic, based upon humans having developed multiple copies of a gene that promotes the easy digestion of carbohydrates thereby increasing our preference.
Is it all genetics? Environment? Lifestyle? A mixture of two of the aforesaid? All three? Sadly, no one knows.
“We eat too much and move too little.”
- David Ludwig, MD, PhD, Professor of Pediatrics and Nutrition, Harvard
While experts are divided on causes and solutions for obesity, most agree that weight gain is a function not only of caloric excess but a reduction in energy expenditure, reflecting decreased activity, in Dr. Ludwig’s words, “with the prevailing wisdom focused on ‘energy balance.’”
In other words, couch potatoes gain weight. At the end of the last century, those with weight problems were called out for being TV-driven couch potatoes. Today, smartphone doom-scrollers earn this critique. Increased consumption of social media (another addiction) reinforces sedentariness, a phenomenon that escalated during COVID-19, which kept people home-bound, locked down, and isolated (and maybe depressed, another possible food consumption trigger). Teens are particularly affected by social media. The CDC reports over half spend 4 hours a day on their phones, and a recent report in JAMA finds teens on their phones for more than an hour during school.
Fatty Liver
The prevalence of non-alcoholic fatty liver disease (NAFLD), renamed as metabolic dysfunction-associated steatotic liver disease (MASLD) in children and teens, albeit rare (affecting one in ten children), has indeed increased (by about 1.35% per annum over the past three decades). This temporal factor suggests we should focus our causal inquiry on secular trends that began in the 1990s.
“If you have hepatitis C your chances of developing fatty liver disease is higher than developing the disease by itself. According to the data, about 50% of people with hepatitis C also have fatty liver disease.”
- Rohit Satoskar, MD, a liver transplant specialist at MedStar Georgetown University Hospital, Washington, D.C
Among several alternative causal factors gaining prominence in the 1990s is hepatitis C (HPC). This viral disease affects the liver and is a 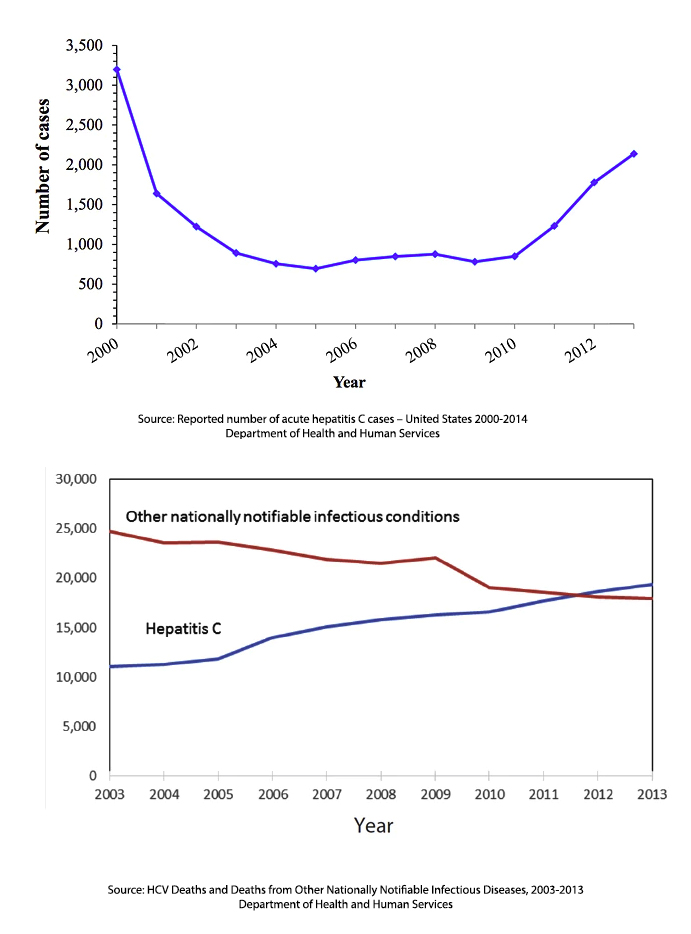 known independent, as well as contributing cause of fatty liver. Hepatitis, a blood-borne infection, can be transmitted through tattoos, razors, and even toothbrushes, as well as contaminated needles facilitated by opioid abuse. However, for children and infants, the most common route of infection is maternal transmission during childbirth.
known independent, as well as contributing cause of fatty liver. Hepatitis, a blood-borne infection, can be transmitted through tattoos, razors, and even toothbrushes, as well as contaminated needles facilitated by opioid abuse. However, for children and infants, the most common route of infection is maternal transmission during childbirth.
HPC is on the rise and has been for a few decades. From 2010 to 2014, infections increased 250%, although it left its mark at least a decade earlier. Since 2012, there have been more deaths due to hepatitis C than all 60 of the other reportable infectious diseases combined. The increase is continuing (doubling since 2014), with the highest prevalence being in those of child-bearing years.
Its implication suggests that studies addressing obesity and UPF should control for HPC exposure by children and their mothers.
Aspartame
The holy grail of the diet-conscious and one presumed antidote to sugar-induced obesity is artificial sweeteners, notably aspartame. Yet, aspartame has been implicated in obesity, notably increasing visceral and skeletal muscle fat tissue, the worst kind.
In fact, a direct link was found between diet drinks and fatty liver disease in a recent study that did control for cigarette smoking but not UPF consumption or exposure to HPC. The postulated biological mechanism for fatty liver disease relied on past studies showing “that diet soft drink consumption is associated with increased body mass index (BMI) and percentage body fat in adolescents.”
“In other words, diet soft drinks that emphasize zero calories may not necessarily prevent weight gain, on the contrary, excessive intake may also lead to obesity. Whereas obesity will bring a series of metabolic problems, so diet soft drink consumption may also increase the risk of metabolic syndrome.”
Multicausal Risks and Societal Actions
Further, food category (i.e., protein, carb, fat) may matter more than its processing, according to Dr. Ludwig, who advocates higher fat consumption as a means to prevent obesity, a contention supported by data on sugar consumption.
Our present knowledge suggests that obesity is not solely caused by UPF. The evidence tying UPF to juvenile metabolic diseases is even weaker. To determine the proper public health policy response, prudence dictates determining how much disease would be prevented if we regulate, limit, or control UPF consumption. This is called attributable risk (AR), defined as “the proportion of disease that can be attributed to a particular exposure .”In other words, the AR estimates how much of an illness is caused by a particular risk factor. Without making this calculation, it is impossible to determine if the costs of regulating UPFs would prevent enough disease to warrant the restrictions.
Will removing/limiting UPF consumption markedly dent the obesity/metabolic crisis in an increasingly sedentary society? As more causes are detected impacting metabolic disease and the incidence of obesity, the proportion of risk attributable to UPF decreases along with the impact resulting from controlling/limiting UPF consumption—translation: More regulation with little to show for it.
[1] While we deflect our energies on UPF
- Over 28,000 Americans died from flu last season
- An estimated 10.3 million cases of measles were reported worldwide, with 285 cases in the US (most unvaccinated).
- Increasingly, states are looking to beef up school vaccine exemptions, with disastrous results expected. One study found children exempt from vaccines were 22.2 times more likely to acquire measles and 5.9 times more likely to acquire whooping cough than vaccinated children.



